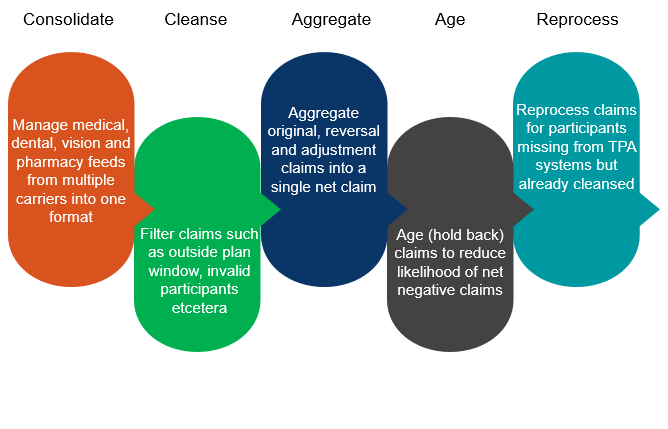
XO® consolidates different formats of medical, pharmaceutical, dental, and vision claims from multiple healthcare insurance carriers into a single TPA-specific electronic data file for claims adjudication and debit card validation. CXC Solutions works closely with TPAs to understand the type of file format that integrates most easily with the TPAs current benefit management system. This single format is customizable to the TPA or can be produced in an industry standard format such as those supported by PowerPlus, BPS, and Lighthouse1. CXC always works to offer a customizable solution that integrates easily with existing systems.Moreover, CXC works to increase the accuracy of claims processed by offering data cleansing and filtering services. Often the lag between enrollment into a carrier system and enrollment into a TPA system, will allow for invalid claims to pass through TPA systems. CXC has the ability to filter out claims from invalid participants and invalid employer groups as well as claims that do not fall within the plan-year. CXC also supports the complexity of grace periods and run-out dates.
Carrier feeds typically contain new claims in addition to reversals and adjustments.XO® has the ability to distinguish between different claim types and aggregate each different claim type reducing the processing work on the part of the TPA. This aggregation process also gives CXC the ability to reduce and manage under/over payments.Although XO® aggregates these claim types, we continue to maintain claim data at a granular level (Deductible, Co-Pay, Co-Insurance, Not Covered, Over & Beyond) and support complex HRA plan designs.
Due to the nature of carrier claims processing, adjustments and reversals tend to arrive long after the original claim has been processed and the TPA has paid the participant. In fact, 96% of adjustments arrive a week after the original claim has been processed while 98% arrive within two weeks.XO® provides the ability to age (hold back processing) claims to help reduce the likelihood of negative net adjustments.
Due to processes in the health insurance industry and the time lag between enrollment in a carrier plan and enrollment in a benefit plan, a participant's valid claim may get filtered out if he is not yet enrolled in the TPA system.XO® has the ability to 'reprocess' claims once the TPA completes the participant's enrollment in their system. This competitive advantage ensures that all claims are processed and that no claims are left behind or lost due to gaps in the enrollment process.
HRA, HSA, and FSA funds all have unique strengths that have become increasingly more appealing with the rising costs of healthcare. As employers look for creative healthcare insurance solutions for employees, many employers have started combining these accounts to provide their employees with creative, inexpensive health insurance solutions. However, as these plans become more complex and require reimbursement from multiple accounts, TPAs need the ability to ensure reimbursements are made from the correct funds.CXC has the ability to support claims feeds for multiple systems (i.e. when one benefits system/TPA manages the HRA plan and a second system manages the FSA plan).XO® can help facilitate the data movement to determine the correct reimbursement cadence and provide this information to the TPA for efficient and accurate claims reimbursement.
XO® provides TPA account managers and customer services teams with an easy-to-use web portal. This web portal provides 24/7 visibility to the status of claims being processed and the receipt of claim feeds from carriers. It allows TPA customer service teams to provide participants with real-time answers to their queries creating a better overall customer experience.